An Interview with Brian Ilfeld, MD, MS
Ultrasound Guided Percutaneous Peripheral Nerve Stimulation
A: Our ultimate goal is to bring a new type of pain control method for our patients, and hopefully that method will outlast the duration of surgical pain and be potent enough so that patients will have essentially a pain-free postoperative experience. If we’re successful, anesthesiologists, surgeons, and patients will have access to a very potent pain control method with essentially no side effects, although there are always risks to every medical procedure.
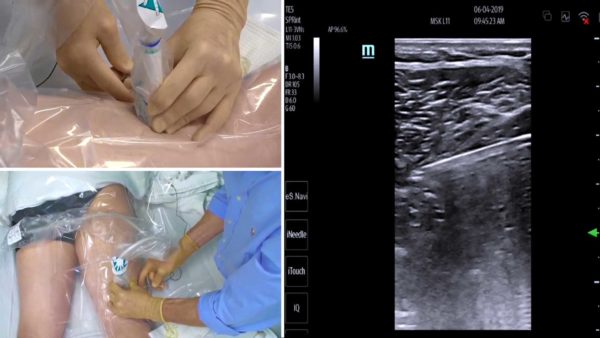
A: Ultrasound-guided peripheral nerve stimulation uses a tiny lead that’s smaller than a piece of thread (0.2 millimeters in diameter) that targets the nerve servicing the part of the body where surgery will take place, with the ultimate goal of a pain-free post-operative experience without the need for opioids, which have some nasty side effects. The lead is placed the exact the same way as a peripheral nerve block or a perineural catheter—we numb up the skin; place a needle through the skin, towards the nerve—but then we use an ultrasound machine that allows us to place that tiny lead right next to the target nerve. We remove the needle lead and that leaves the lead in place. It’s so small people cannot feel it and a Band-Aid basically holds it in. When patients come into the recovery room, we then stick a small stimulator to the body with an adhesive pad so there’s nothing for the patient to carry and no local anesthetic or infusion pump required postoperatively. Patients go home for two weeks with their lead in place, and when they come back for their two-week postoperative check with their surgeon, the surgeon simply removes the Band-Aid and pulls on the lead and the lead slips out. It keeps it simple for the patient.
Through our trial, we are hoping that the following questions are answered: How much pain control does it provide, if any? Does it decrease side effects from opioids, such as nausea or vomiting? Does it improve pain control? Does it improve sleep? So, these are some of the things that we’re hoping this technique will bring for our future patients.
Now because it’s a study, patients are randomized, just like a flip of a coin. Half the patients receive active stimulation in the recovery room, and half the patients receive a stimulator that’s a sham. It doesn’t help. It doesn’t hurt. It means that at the end of the study, we’ll have two groups, and one group received our standard of care, which is a single injection nerve block, which lasts about 12 hours, plus pain pills at home as they need it. The other group received that same standard of care, plus the stimulation, so that way we can see what stimulation brings, in addition to what we’re already doing.
A: Opioids, and other pills used for pain control, have some very nasty side effects, such as nausea, vomiting, and sedation. They can be dangerous in some groups of patients, especially very elderly patients, not to mention the risk of addiction or overdose. The technique essentially has no side effects whatsoever. In fact, most of our patients don’t even realize that the stimulator is on since they usually don’t feel much at all. Additionally, this technique can also be used in conjunction with other types of pain control methods, if needed.
This technique should benefit our veterans, our active duty members, and their family members by reducing post-operative pain in some of the most common surgical procedures done the world over. Our hope is that by decreasing the amount of pain that people feel, it will increase their ability to participate in rehabilitation. We know that one of the major limitations with rehabilitation is pain, and people simply don’t want to move the joint affected by the surgery, so it’s difficult to do physical therapy if you don’t move the affected part of the body.
While that has never been conclusively demonstrated, we anticipate that the experience of less pain with less side effects will provide our patients with potent pain control in the first two weeks post-operatively. We’re also hoping that treating acute pain initially will then decrease the risk of developing chronic pain, which is a risk for all surgeries.
A: This FDA-approved technique is applicable to almost any surgery, but primarily best for surgeries where the surgical site is innervated by one, or at most, two, major nerves. The tiny leads that we place work very well for large nerves, such as the femoral nerve or the sciatic nerve, but don’t work as well where you have multiple nerves, such as surgical procedures of the chest because there are different, small intercostal nerves between the ribs and that single lead cannot affect all of those different intercostal nerves.
Ultrasound-guided peripheral nerve stimulation is approvable for chronic pain and acute pain; however, it’s never been studied in acute pain or postoperative pain, and so, that’s why we’re now doing this trial. The surgical procedures that we’re using this for are major shoulder surgery, such as rotator cuff repair, and major foot and ankle surgery, such as ankle arthrodesis, or a bunionectomy. We’re studying bunionectomies specifically because they reliably result in a good deal of pain. We are now in the pilot study looking at knee surgery, such as ACL repair; however, in the PMC study, we probably will not be including the ACL repairs because there are two major nerves that innervate the knee and we’re using a single lead for this study.
A: Peripheral nerve stimulation was proposed back in the 1960s. At that time, didn’t have a particularly good way to get the electricity, or the current, to deeper nerves. We had only leads where you had to open up the skin, cut down to the nerve, expose the nerve, and then place the lead around the nerve itself, and then sew everything back up. So, you can see that’s a major procedure in and of itself, and it’s risky in many ways, especially for nerve injury. Not only that, but after using it for a couple of weeks or months, fibrosis occurs. While that’s the body’s way of trying to heal itself, in this case, the fibrosis occurs with the lead attaching to the nerve itself and so when the lead is removed, you have to essentially cut or pull this lead off of the nerve, which can induce injury in itself. So, it was really used only as a last case resort for chronic pain for the last 60 years.
About 30 years ago, the first percutaneously inserted leads were introduced—that’s where we can place a needle through the skin that has been numbed, place the lead through the needle, and remove the needle, leaving the lead in place. This procedure has been looked at for primarily intramuscular use or spinal cord use, and used for chronic pain during this time. It wasn’t till about 10 years ago, that people started looking at perineural use using the percutaneous or the through the skin technique. While we’ve been looking at this technique to treat chronic pain, we now want to look at it in acute pain or postoperative pain model. They are different—causes of chronic pain and causes of acute pain are usually separate. This technique is approved for use by the FDA for both chronic and acute pain, so it is not an experimental technique per se. What we’re doing now is specifically looking to see, does this technique bring benefits to our postoperative patients? If so, what are those benefits? And also what are the potential side effects and risks?
We can use TENS [transcutaneous electrical nerve stimulation] units, which deliver small electrical impulses through electrodes that are attached to the skin with adhesive pads. The problem with TENS is that if you increase the current enough to affect the deeper nerves, it hurts on the skin too much. So, there’s a limitation of how much current TENS can actually use. What we need to do is bypass the skin with the PNS lead so that we can introduce the current directly to the nerve, and bypass the skin completely.
Videos & Other Information
Video: Ultrasound-Guided Peripheral Nerve Stimulation for Postoperative Pain Management
Video: Ultrasound-Guided Peripheral Nerve Stimulation for Postoperative Pain Management Brian Ilfeld, MD, MS, talked with the Pain Management Collaboratory Coordinating Center about his pragmatic clinical...
Read MoreUltrasound Guided Percutaneous Peripheral Nerve Stimulation: A Nonpharmacological Alternative for the Treatment of Postoperative Pain (Ultrasound Guided PNS trial)
This trial, determines the effect of a novel, nonpharmacologic analgesic technique—percutaneous peripheral nerve stimulation (PNS)—on postoperative analgesia and opioid requirements, as well as physical and...
Read More